
Often described as a cruel mystery, the word ‘Lupus’ carries a heavy weight for many. This unpredictable autoimmune disease presents unique challenges for people with it.
This unpredictable autoimmune disease presents unique challenges for people with it. Your body’s defense system, called the immune system, mistakenly attacks healthy tissue. This attack causes widespread inflammation in the body. It might affect joints, skin, kidneys, and even your brain sometimes. Imagine living life when your body turns against you like this.
Symptoms sometimes mimic other conditions, making them hard to spot early. This situation is why getting a diagnosis frequently takes years. Brave public figures have stepped forward, sharing their journeys with lupus. These stories help other people feel less alone and more understood.
Actor Chhavi Mittal, a survivor of breast cancer, lately spoke out. She shared a personal story about her lupus rash coming back again. Posting photos of arm spots on social media felt truly resonant. Chhavi was honest about feeling like things weren’t in her control much. Many people facing chronic illness can relate to these feelings deeply.
She wrote, “My lupus rash keeps returning even though I try hard.” It frustrates her since she doesn’t know what causes these flare-ups to happen. Chhavi’s experience shows a common and hard part of lupus – unpredictable flares. The lasting impact they leave is also a significant struggle. She noted having many spots on her body without knowing why. This lack of clarity stays even after getting medical advice from doctors. Trying different treatments, including old steroid use, seems unhelpful for her.
Her story speaks to the difficult nature of controlling the disease. Despite health struggles, Chhavi reminded followers to always count their blessings. Halsey, a singer, is another brave voice in the lupus conversation now. Only 29 years old, Halsey recently announced her diagnosis to the world. She shared personal footage, offering a glimpse into her health journey at home. Halsey remarked in one video, “I feel like an old lady,” massaging her legs frequently.
This feels relatable for others dealing with pain and fatigue from lupus. Halsey’s determination shows through as she hopes for a “rebirth” someday. She looks forward to redoing her twenties in her thirties with energy and good health finally. Sharing her private battle aligns with releasing her new music for fans. She described herself as feeling lucky to be alive after her health issues. Halsey wrote an album during this period, turning her experience into an art form.
Her history with health problems, like endometriosis, shows links between health issues. She mentioned her body felt like it was rebelling after childbirth sometimes. Halsey uses her platform to raise awareness by tagging organizations online. Selena Gomez also discusses her life with lupus openly. She has helped educate many people about this condition and its challenges.
Diagnosed in 2013, she told the public in 2015 after chemotherapy treatments. She shared the impacts of rumors about her health, emphasizing the toll on mental well-being. “I wanted very badly to say, ‘You guys do not have any idea. I’m in chemotherapy’,” she said later. Selena’s explanation showed why she withdrew until she felt more confident inside. Her story highlights how managing chronic illness also involves public perception.
Selena’s journey also shows the potential severity of lupus symptoms. She admitted ignoring early symptoms like fevers and fatigue for a while. Pushing through despite them felt like the wrong choice looking back now. She stated later, “I do not think I made the right decisions because I didn’t accept it properly.” “And that’s extremely selfish acting, and at the same time, very unnecessary.” “I’m not really proud of that time period looking back,” she confessed about it.
Her experience reminds everyone to listen to their body signals always. The path of lupus felt unpredictable and led to a critical point for Selena. Her diagnosis reached a stage doctors call “life or death” sometimes. A kidney transplant became needed in 2017 due to a complication from lupus. This serious condition called lupus nephritis happens when lupus attacks the kidneys hard. It stands as a leading cause of death for people who have lupus in the world.
Selena explained that her doctors told her about lupus nephritis after constantly monitoring her kidneys. She required a transplant because of it, which was a hard thing to face. Medical experts like Dr. Emmanuel Katsaros stress the need for regular kidney checks. They often recommend that lupus patients see a rheumatologist regularly for monitoring. Often, patients have no early signs that their kidneys are affected until more damage occurs. This is why consistent check-ups feel essential for patient care. Selena’s friend, Francia Raisa, donated a kidney bravely to save her life.

We move past personal stories and explore lupus from a medical perspective today. Doctors sometimes find diagnosing this particular illness very difficult. Lupus presents with many symptoms that create great confusion. These signs often resemble other severe health conditions. This confusing similarity makes diagnosis incredibly tricky. Patients also struggle significantly to obtain a correct diagnosis.
Medical professionals often refer to lupus as “the great imitator”. This specific nickname is certainly well-deserved by this disease. Its varied symptoms often closely resemble those of many other diseases. This causes much confusion and delays patients’ accurate diagnosis. Understanding all its signs helps solve this puzzle. Doctors need to know the conditions that it mimics.
One very tricky aspect is related to SLE, which is lupus. It often overlaps significantly with Kawasaki disease, known as KD. Both diseases result from the body’s immune system attacking. They can present with vasculitis, which means swollen blood vessels. In lupus, immune complexes frequently deposit in vessels. Some people develop vasculopathy without these deposits being present.
Studies of patients show how these illnesses look quite alike. Sometimes they even occur together or are misdiagnosed. Doctors apply certain rules for diagnosing KD and SLE. But the many variable features make this process challenging always. It gets especially hard when cases are not typical. It is also tricky if symptoms strongly overlap.
We see three patient cases illustrating this difficult diagnosis process. Case 1 was a boy, who seemed to be sixteen years old. He had a fever, headaches, abdominal pain, rashes, and swollen glands as well. The first diagnosis doctors considered was KD. But then he developed seizures and brain problems later. Skin tests plus the finding of specific antibodies indicated it was actually lupus.
This patient showing signs of both illnesses surprised few. Doctors discussed whether it was both diseases occurring or simply lupus affecting the heart at times. Other doctors have reported similar cases recently. This case proves that a patient’s condition can change rapidly sometimes. Many different tests plus observations helped achieve a proper diagnosis.
Case 2 was about a boy, who I think was twelve years old. He went to the hospital, with doctors suspecting lupus. He showed symptoms of fever, joint aches, hair loss, rash, and mouth sores. His blood tested positive for ANA as well. But later examinations revealed red, peeling skin on his hands and feet. They also noted redness near the groin area. High liver enzyme levels and heart scan abnormalities pointed to incomplete KD.
Receiving treatment with IVIg, aspirin, and steroids seemed to work. His heart and liver problems improved significantly after this. This strongly supported his diagnosis of atypical KD in the end. This whole case shows that symptoms can initially change rapidly. Or signs of one illness can appear alongside those of others at any time. Doctors need to be flexible and use a broad diagnostic list as well.
Case 3 concerned a girl, who I guess was eleven years old. She first showed symptoms very similar to typical lupus: swollen glands, arthritis, a facial rash triggered by sun exposure, and dark urine. She also had a persistent fever. Her lupus diagnosis was based on several factors: acute skin lupus, joint pain, kidney involvement, and blood abnormalities. These included low white blood cell counts, a positive ANA test, and a positive anti-dsDNA test.
While she was in the hospital, her fever persisted. She developed red, crusty lips and a spreading body rash. Her hands and feet turned red and sometimes peeled severely. Doctors administered IVIg, thinking she might have a Parvovirus B19 infection. That virus can sometimes truly mimic the specific illnesses they found. Later imaging revealed large swelling in her heart arteries. This is often associated with severe KD cases, they noted. However, artery problems can also occur in other vasculitides, including lupus at times.
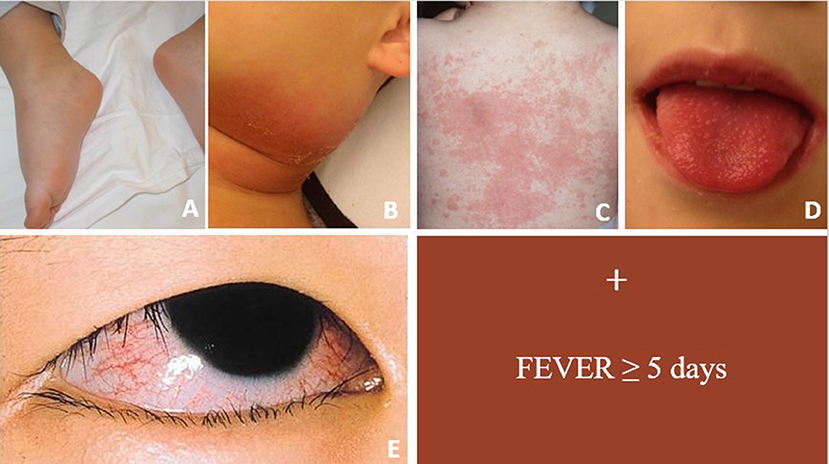
Discussing these cases shows that KD and lupus share signs. Fever, swollen glands, and arthritis often occur in both. Eye and mouth issues also appear, as well as a rash. Both illnesses quickly affect many body systems. Having both or a misdiagnosis by doctors is challenging. This presents a big challenge for teenagers today, who may show unusual KD or perhaps some lupus signs.
Both diseases can appear together or with years in between. An illness called JIA can also cause heart artery swelling. This just makes diagnosis much harder for doctors. Doctors must check everything accurately and thoroughly. This ensures that patients receive proper treatment right away. It helps minimize problems much later on.
Finding lupus itself is complex even when considered alone. It is not just about overlapping with KD. There is never a single simple test for lupus. Doctors often start by ordering blood tests first. They look for antinuclear antibodies, always referred to as ANA. This checks if the body’s defense system is highly active.

An ANA test is often positive for people with lupus. But having a positive ANA test does not prove lupus. A positive ANA result can occur in other conditions as well. Even healthy people sometimes show this positive result. Doctors therefore gather information from multiple sources. Patient history, physical exams, and other tests are greatly important. Sometimes doctors even take a tissue sample.
Finding protein or blood in urine is also important. This often indicates kidney problems associated with lupus. Kidney issues occur frequently and can be very serious. But patients may not always show clear signs. Kidney damage might be quite advanced before symptoms fully appear. So doctors must consistently test urine, I believe.
Many different symptoms make diagnosis quite difficult. Joint pain and swelling commonly occur with lupus. But this can easily be mistaken for an injury or overuse. The classic butterfly rash on the face is well-known. But not all lupus cases have this rash. It can sometimes resemble the skin condition rosacea. Other rashes, like discoid rash, are also sometimes misidentified.

Also, lupus patients often experience many symptoms, such as extreme fatigue, hair loss, and fingers changing color when cold. These symptoms are not always on the official lupus list. People without lupus can also easily experience them, it seems. These less specific signs make diagnosis very complex indeed. It is harder to distinguish lupus from general health problems.
What causes lupus is still being researched very hard. But much progress has been made recently, doctors find. Experts believe that a combination of factors always causes lupus. A genetic predisposition seems to be present in many cases. This is called the “first hit” by some specialists. Autoimmune diseases often run in families, you know. But they can appear very differently among relatives sometimes.
After the genetic setup, the environment plays a big role. Some environmental factors can trigger the illness later. This is often called the “second hit” by doctors. Triggers include certain viruses, sunlight, or UV rays that activate the immune system. Hormones also matter since most patients are women, and symptoms often flare near periods or during pregnancy. Figuring out the exact interaction of factors is now the focus of research.
A cure for lupus remains the ultimate goal, you know. But it is much more treatable now than it ever was. This is because we understand the immune system’s response better. Current treatments focus on reducing inflammation quickly. They aim to prevent long-term organ damage entirely. This can be truly devastating if left unchecked.
One medication often used for lupus treatment is hydroxychloroquine. Doctors consider it a very important cornerstone indeed. It is generally regarded as relatively mild, they say. It typically has limited side effects as well. But long-term usage requires monitoring for potential eye toxicity. For many patients, however, hydroxychloroquine alone is not enough. It fails to control the disease effectively for them.
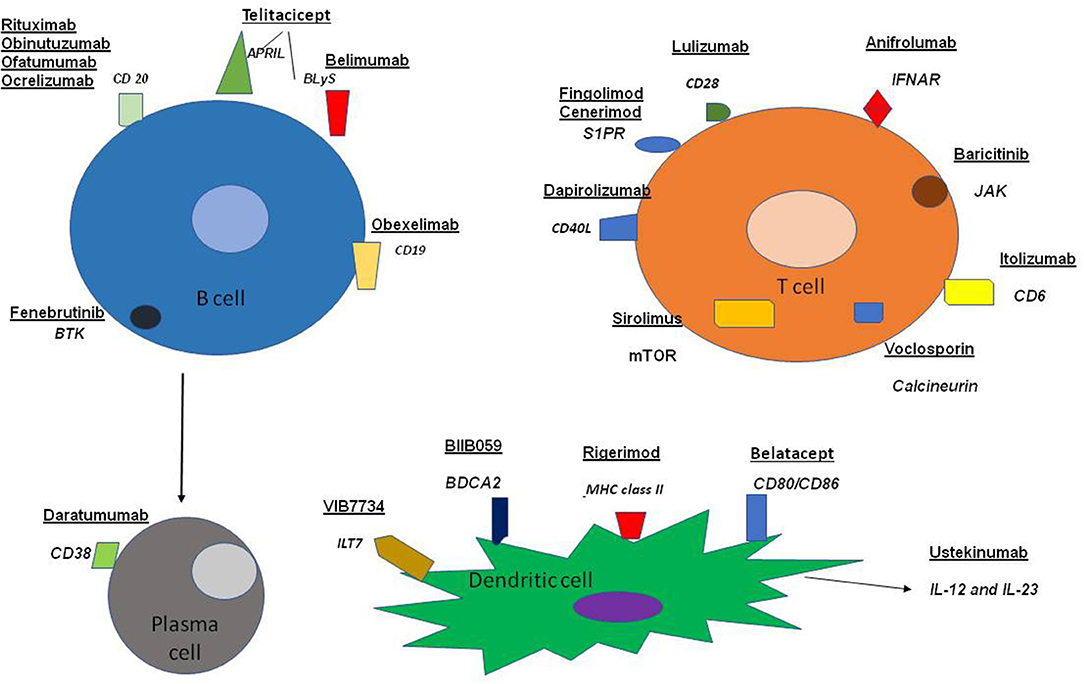
Sometimes stronger immunosuppressive medications are needed. These are effective at suppressing the entire immune system. But they usually bring a risk of infections. This is because their impact is too broad. So doctors need more targeted ways to treat. These would quiet only specific problematic parts of the immune system. They would not harm the overall immune function as much.
Exciting research is actively developing more targeted therapies. The goal is to create medications specifically for lupus immune processes. This might lead to fewer side effects for patients. It is better than the broad immunosuppressants used now. A few targeted medications have recently gained approval. Many more are currently being actively developed. This brings substantial hope for future lupus treatment.
Beyond targeted therapies, small studies also examine remission. This means that patients might be able to stop taking medication entirely, often without the sickness becoming active again. This research is still in its early stages. But it fuels optimism that a cure might be near soon. Long-term remission could indeed be possible someday.
Managing lupus effectively involves avoiding flares. Flares disrupt daily life greatly. They can also sometimes lead to permanent organ damage. Protecting yourself from sunlight exposure is crucial. UV exposure can greatly activate the disease process. This requires diligent sun avoidance plus consistent use of broad-spectrum SPF.
Getting up-to-date vaccines is another important step. Infections can definitely trigger the body’s immune response severely. This might quickly start the autoimmune process. Research on gut health and diet is still ongoing. Avoiding emotional and physical stressors is generally advised. This helps minimize flares for lupus patients.
Lupus is unpredictable, I always see. One day, symptoms feel very significant, and the next day, they feel okay. This indeed requires much adaptability and resilience from patients. Historically, lupus greatly impacted life expectancy. But advances in treatment mean less life-shortening now. Lupus should not significantly shorten a patient’s life anymore today.
Focus is now mostly on managing other health issues. Secondary problems are more common in patients with lupus. Heart disease is now recognized as an important area to watch closely. Experts emphasize that the exact cause of lupus remains unknown. Multiple factors contribute greatly to the development of the sickness.
Patients, doctors, and family working together help. This collaborative effort is seen as key to managing symptoms. It may help achieve remission for some. It allows individuals with lupus to live full, long lives today. The journeys shared show the challenges faced always, but also remarkable progress in understanding this sickness. This propels hope for continued advancements quickly.
Related posts:
Chhavi Mittal shares struggle with Lupus Rash: Doctors are failing at advising
A Teenager With Rash and Fever: Juvenile Systemic Lupus Erythematosus or Kawasaki Disease?
I’m a doctor — beware this ‘cruel mystery’ disease that can permanently damage organs




