
Cancer is often linked to old age. Many people think it happens late in life. But a quiet shift is happening now, especially with cancers in your stomach and bowels. It isn’t just an old person’s problem anymore. Data shows more young adults get diagnosed. This changes old ideas about symptoms.
A stark picture emerges from the numbers. Colorectal cancer affects the colon and rectum. A recent study finds it leads cancer deaths for men under 50. For women that age, it is second now. This was the fourth cause before. The health landscape is changing fast. Serious threats enter prime years.
The trend isn’t only colorectal cancer. It shows in many GI tract areas. Appendix cancer rises sharply in Gen X and millennials. An analysis looked at nearly 5,000 cases. Gen X adults had over three times more incidence. Millennials’ rate was four times higher.
Dr. Andreana Holowatyj leads the study. She finds it concerning that rates triple and quadruple. But she stresses the disease is rare overall. Still, malignant appendix tumors more than doubled. This happened from 2000 to 2016. The biggest increases were seen in younger groups.
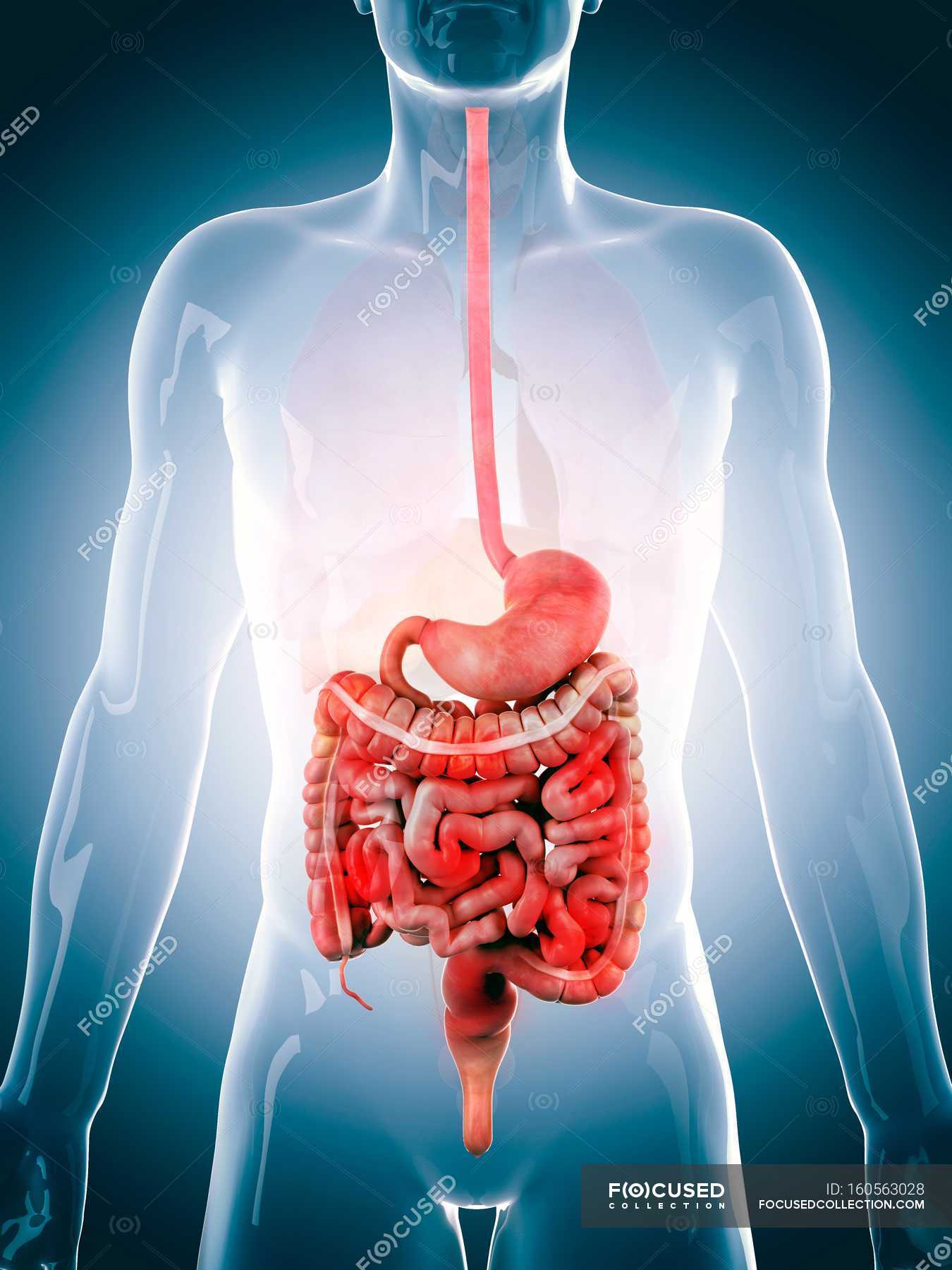
Dr. Holowatyj says this pattern isn’t limited. “This is not just cancers of the appendix,” she states. “We’re seeing a trend across multiple GI cancers.” Her lab focuses on early-onset cancers, diagnosed before age 50. The rise is visible in the stomach, pancreas, and esophagus too. This troubling wave impacts the digestive system.
Amid the statistics are personal stories. Like Heather Barry’s difficult journey. She is a young mother. In September 2023, she just had her third daughter. Heather knew something felt wrong in her body. She recovered from delivery, but symptoms appeared.
She started struggling with constipation. Then she noticed blood in her stool. These felt like clear body signals to her. She told her OB-GYN in September. The doctor thought they were postpartum symptoms. Advised stool softeners and diet. “She reassured me,” Barry said later. “She even said give it a year.”
This first reassurance proved frustrating. It was the start of a delayed diagnosis path. Later that month, a physical exam brought similar results. The physician did not flag symptoms as serious. Yet the problems did not stop. They got worse instead.
She ate less food than before. Extreme discomfort troubled her days. She continued seeing blood whenever she used the bathroom. October brought another attempt to find answers. She saw a colorectal surgeon then. The surgeon diagnosed hemorrhoids as the problem. Recommended the usual remedies again.
Heather felt increasingly desperate. “I felt like I was on a hamster wheel,” she shared. “People kept telling me you’re OK. But I knew I wasn’t well.” The situation turned critical as she was losing weight. She shed 30 pounds by the end of October. Taking much Miralax daily just to manage constipation.
No relief appeared for Heather. Her condition kept getting worse. She changed her primary care physician. She hoped for a new perspective this time. Her new doctor also first diagnosed hemorrhoids. The advice remained consistent for her: cream, pelvic floor therapy, and a gastroenterologist referral.
Read more about: The Hidden Cost of Getting It Wrong: How Misdiagnosis Devastates Lives and Strains Healthcare
Seeing the gastroenterologist brought new suggestions. Maybe a hormone imbalance was the issue. But the core recommendations stayed the same. Softeners and high-fiber food were still advised. This misdiagnosis cycle made Heather question herself. “I felt like I was ‘going mental,'” she expressed clearly.
The physical pain was immense. It was especially bad at night sometimes. “I was in so much pain every night,” Barry told someone. “The only reprieve was the shower. I would just lay on the floor.” The emotional toll felt heavy. She felt unheard by doctors. Knowing something was fundamentally wrong. “I felt like I was screaming,” she described, “and nobody was listening.”
A turning point finally arrived. In December, she started pelvic floor therapy. The physical therapist saw her condition firsthand. Alarmed by the severity of the symptoms she saw, the therapist helped secure another expert appointment. This led to a test for her bowels. It showed dysfunction there.
This finding validated her concerns. It was a crucial step forward. In January 2024, she saw a different gastroenterologist. This visit led to a colonoscopy and an endoscopy procedure. Waking up from the procedure, the atmosphere felt different.
Read more about: Starbucks’ Bold Olive Oil Coffee Brew: High Hopes Meet Unexpected Customer Reactions
“I was barely woken up,” Barry recalled. “Everybody was moving really quickly around me.” The doctor’s words confirmed her fear. “You need to go now,” he said. “We need to send you to the colorectal surgery department. He was 99% sure about cancer.”
Minutes later, the diagnosis came. Official: Stage III colon cancer. She was just 34 years old then. Heather Barry’s difficult journey is common. Many young adults face GI cancers. Dr. Ted Hong treated Barry. He is the director of GI radiation oncology. Her struggle for diagnosis is not unusual.
“New phenomenon of younger patients,” Hong explained. “Having colorectal cancer is not on most doctors’ radar.” This highlights a systemic gap. Awareness and suspicion are missing for younger people with common symptoms. These symptoms are often linked to less serious issues.
Cancer symptoms can be vague initially. It’s easy to confuse them with minor problems. Dr. Zachary Brown is a surgical oncologist. He points out appendix cancer symptoms. “Symptoms are vague, nonspecific,” he notes. “They often overlap with other cancers.”
This overlap contributes significantly to delays. Patients might have persistent abdominal pain. Fatigue can be present too. Unexplained weight loss sometimes happens. These are easily dismissed as stress or diet changes, common ailments. Because of the non-specific nature of symptoms, they are often found late. This challenge is seen across early GI cancers.
The list of symptoms is long. Unexplained weight loss is a red flag. Losing over 10 pounds without trying signals several cancer types. Constant fatigue is another symptom. It persists even after rest and can interfere with daily life tasks. It’s easy to dismiss but warrants looking into.
Changes in appetite can be a symptom. Eating less, feeling full fast happens with ovarian cancer sometimes. It also occurs with conditions not in the reproductive system, demonstrating symptomatic overlap and confusion. Persistent indigestion or nausea is common too. It’s usually linked to ulcers or acid reflux but might signal gynecologic cancer instead. It shows how symptoms are misleading in the abdomen area.
Pain in the pelvis or abdomen frustrates doctors most. Ongoing discomfort means many things. Gas, indigestion, pressure, bloating, cramps occur, usually due to gut issues or hormones. But it could signal ovarian or endometrial cancer. Critically, it’s tied to colon cancer like Heather’s. Doctors advise paying attention if pain lasts over two weeks.
Changes in bowel habits are key. This is relevant for colorectal and appendix cancers. Alterations in size or shape happen. The frequency of movements can change. The text highlights pencil-thin poop. Experts say this is a concerning sign if a new and persistent change happens. It could indicate a tumor narrowing the colon passage.
Diarrhea or constipation is different. If previously absent, do not dismiss it. It could signal a tumor pressing on the colon. Even symptoms that seem distinct connect sometimes. Frequent urination or pelvic pressure occurs, often a sign of a UTI problem. If ruled out, it could potentially signal gynecologic cancer.
This underscores the complex symptom interplay. Bloody vaginal discharge is usually a sign of infection or post-menopausal endometrial cancer. It is a common symptom of cervical cancer too and less commonly of vaginal or endometrial cancer. It requires careful evaluation to tell the sources apart.

Challenge lies in symptom subtlety. Dr. Therese Bevers points this out. “Most cancers are asymptomatic at the earliest stages,” she adds. Recognizing subtle changes is crucial now. Advocating for investigation matters, especially for younger people who fall outside the typical screening age.
Exact reasons for the rise are unknown. They are the subject of ongoing research projects. Speculation points to multiple factors. Cancers may share risk factors that we have changed, like obesity and poor eating. Alcohol consumption and tobacco use too. Dr. Ardaman Shergill speculates, “Risk-reducing strategies likely help prevent appendix cancer.”
Stopping smoking is an example. Limiting alcohol and exercising helps. Genetics may also play a part here. Dr. Holowatyj’s lab is working to try to understand how risk factors contribute. The complex puzzle involves lifestyle, environment, and inherited predispositions, which are possibly intertwined.
Ultimately, the rising incidence is a problem. Gastrointestinal cancers in young adults are increasing. Symptoms are nonspecific for many. The lack of routine screening for this age group creates a perfect storm for diagnosis delays. Stories like Heather Barry’s remind us that the human cost of this trend is immense. The difficulty of being heard when symptoms don’t fit the pattern exists. It highlights the critical need for more awareness among the public and the medical community too. Vague symptoms should not be dismissed automatically. Always investigate the potential for cancer. The journey to diagnosis can be long. But recognizing signs helps a lot.
GI cancers are rising in young folks these days. Symptoms for these cancers are sometimes hard to find early. Knowing treatment options matters for patients. The reality of prognosis is part of the journey. Patients advocating for themselves helps a lot. Getting a diagnosis can feel like a tough road. Doctors should try to find it quickly and accurately.
Treating these cancers uses many methods overall. Plans change based on what type of cancer it is. Heather Barry had Stage III colon cancer that she found. Her plan was very aggressive indeed. First, she got a colostomy to help her. This allowed her to eat and eased constipation problems. Then came chemo and radiation for the tumor.
Doctors removed the remaining tumor after therapy was done. She needed another surgery to switch the bag back. This helps her body work more like usual. Surgery for these cancers can take very many hours. Dr. Shergill pointed out how complex it is. Chris Cotton had bladder cancer that spread. He is getting chemotherapy treatment now.
What happens next varies a lot for patients. Prognosis depends on several important factors. The type of cancer you have makes a difference. The stage at diagnosis is another key factor. If cancer spreads, it changes the outlook very much. For appendix cancer, rates vary widely. Low-grade tumors have pretty good survival rates.
Advanced appendix cancers have lower rates, though sometimes. Dr. Brown said knowing tumor biology helps a lot. Better detection can improve future outcomes. Chris Cotton had Stage 4 bladder cancer. It had spread to his lymph nodes, unfortunately. His doctor estimated his remaining time was short indeed. Stage really shapes the prognosis a lot for people.
Getting diagnosed quickly is very important for people. Earlier detection usually leads to better outcomes. But finding it early in young adults is hard. There are no regular screening programs for that age group. Screening normally starts at age 45. This is for adults with average risk, you see.
Family history means you screen sooner typically, maybe 10 years before the relative’s age. Many young adults lack this history, though, unfortunately. They fall outside the normal screening age completely. Heather Barry’s doctor didn’t pursue her questions. She reported no family history herself. Dr. Bevers said early cancers often have no symptoms.
Read more about: Beyond the Bump: Shocking Discoveries Inside Women’s Bodies Reveal the Power of Listening to Yourself
Symptoms are how young people sometimes find cancer. They cannot get routine screening yet, right? But early GI cancer symptoms are vague and unspecific. This makes detection hard for both patients and doctors. Symptoms are like persistent stomach pain or fatigue. Unexplained weight loss is another potential sign. Bowel changes or indigestion can happen too.
Doctors often dismiss those symptoms first off. They think it is IBS or just stress, maybe. Dr. Brown said appendix symptoms overlap with other issues. Dr. Cecchini noted pencil-thin stool sometimes. This can happen if tumors narrow the colon pathway. It could be a concerning sign to watch for, though less common than pain or finding blood.
The problem gets worse for young patients seeing doctors. Professionals attribute symptoms to less serious causes. Early cancer is not on their radar often enough. Heather Barry had many doctor appointments. They blamed postpartum effects or hormone issues for her symptoms. She kept getting the same advice again and again. This misdiagnosis made her feel desperate.
Patient advocacy is very critical now overall. Young adults must push for investigation themselves. Their symptoms get misinterpreted very easily. Heather Barry’s journey had a turning point finally. Her physical therapist got alarmed by her situation. He helped her see another expert fast. This led to tests and her diagnosis eventually.
Heather’s message is strong for everyone, she says. “Push and don’t stop pushing,” she advises strongly. If something feels wrong, you should insist they check. Dr. Hong confirmed patient advocacy is key for young ones. Sometimes you have to bounce around doctors. Chris Cotton had a similar issue with UTI symptoms. He also needed repeat visits before being diagnosed.
Patient stories drive important change overall. They show the human cost of delayed diagnosis. They are a powerful call to action for everyone. This applies to both the public and the medical community. Doctors need awareness of the GI cancer rise in young adult patients. Vague symptoms need prompt investigation. Do not just dismiss them easily by mistake.
Looking ahead, there is a clear path forward. It involves more research work. Increasing awareness helps a lot indeed. We need commitment to early detection challenges. Reasons for the rise are still being investigated now. Risk factors like diet and obesity are suspects. A genetic component could play a role too.
Ongoing research is crucial right now. Raising awareness is also of vital importance. GI cancer is not only for old people anymore. This message needs to spread widely. The public need to know the symptoms to look for. Seek help if symptoms are new or persist for weeks. Doctors need more training on young patient cases.
Diagnosis at a young age is a daunting prospect sometimes. Stories of strength give hope to many. Focus on this trend is growing thankfully. The goal is always to catch cancer early. They are most treatable and maybe curable then. Dr. Cecchini said early detection helps manage the disease state. The majority of people are still cured yearly from this.
Patient journeys show important lessons overall. Listen to your body signals it sends. Advocate strongly for your health yourself. Ensure vague symptoms get investigated. Be informed and be persistent always. Increase awareness and support research now. Empowering advocacy saves lives for people we know.
Related posts:
10 cancer symptoms women shouldn’t ignore
Appendix Cancer Sharply Rises Among GenX and Millennials
Doctors said a 34-year-old mom was experiencing normal postpartum symptoms. She was then diagnosed with advanced cancer




